HEALTH PLANS
Predict risks and costs. Collaborate with providers.
Leverage Claims and Clinical data to accurately identify risk and care for your members. Calculate accurate HCC and RAF scores. Strengthen coding and supporting documentation to have zero-impact RADV audits. Enable a network to improve coding, care coordination, and quality of care.
We can reduce cost of care and manage high-risk members.

Create high-performance networks. Identify at-risk members for early intervention and care management. Reduce risk associated with CMS audits.
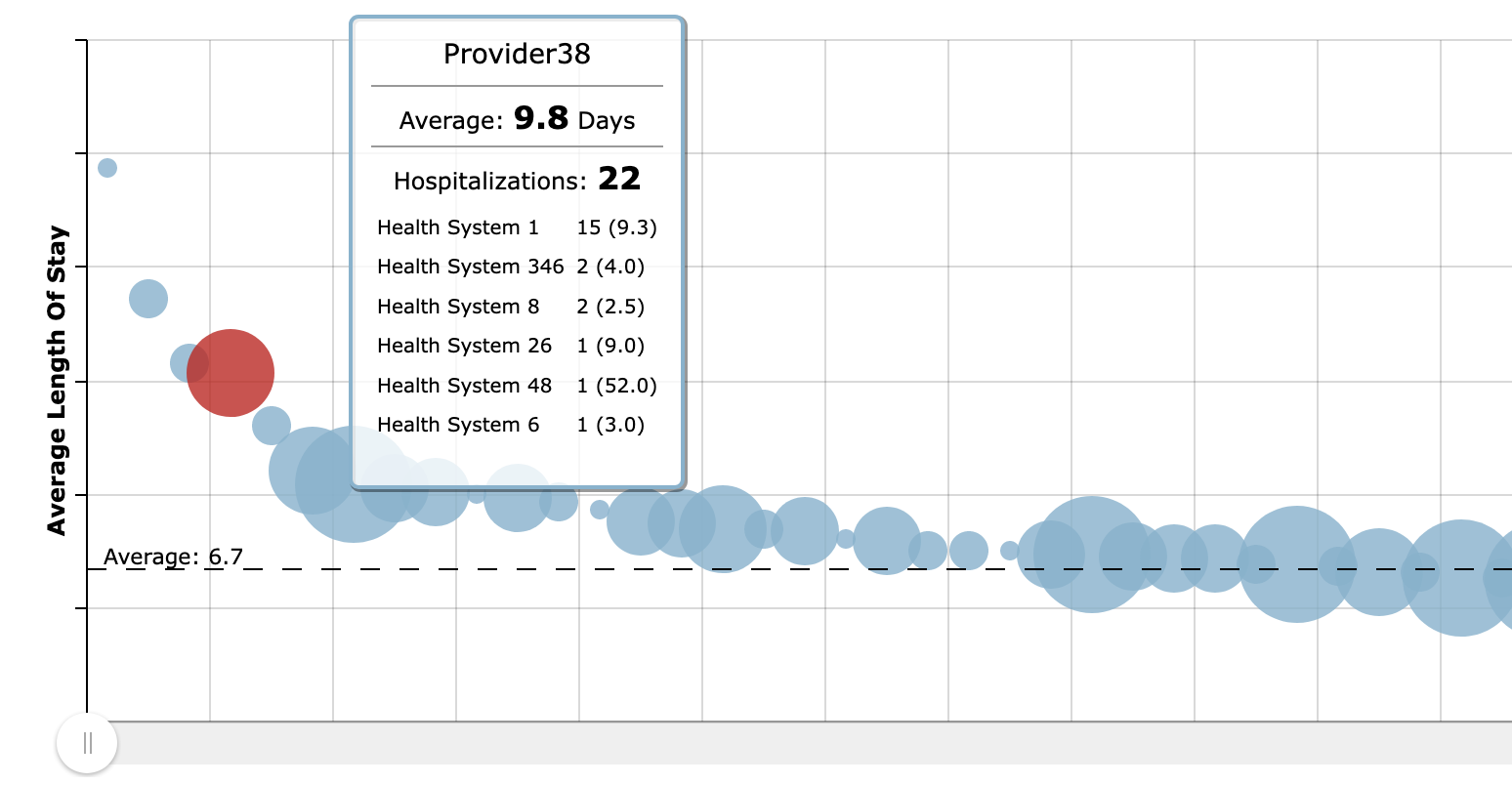
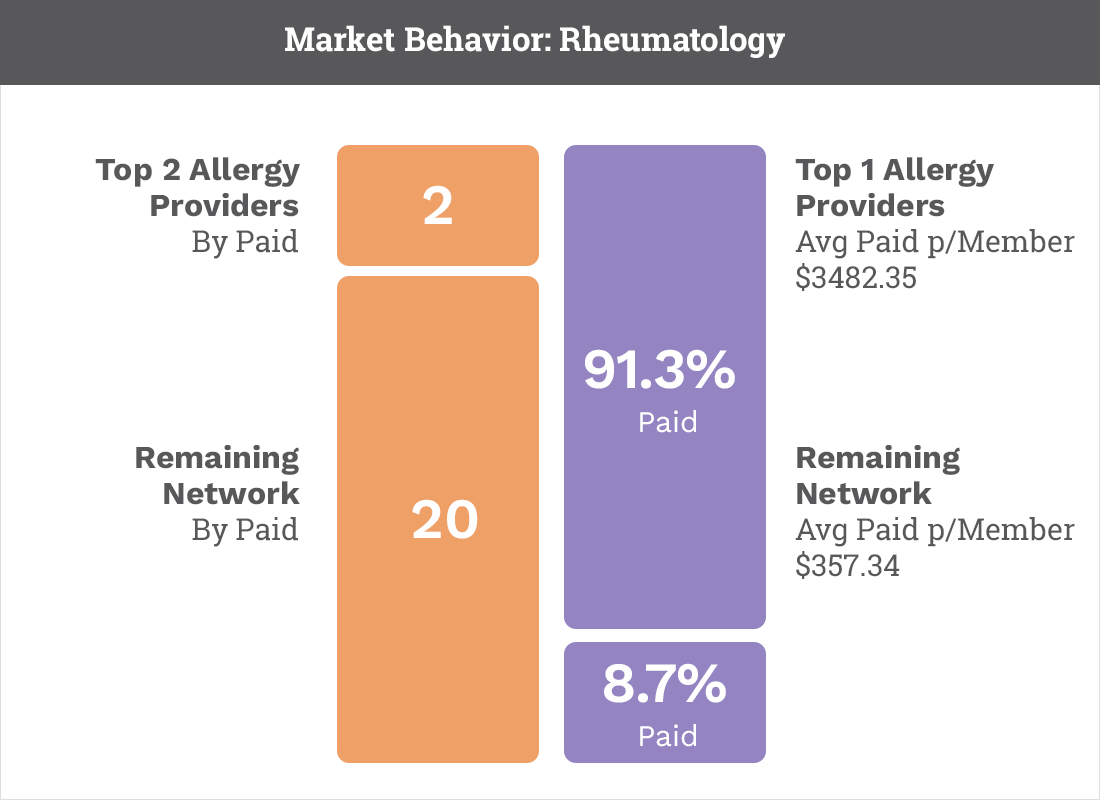
Visualization of Member Care Journey
Create effective system-level interventions and establish patient care coordination priorities.
Clinical Data Distribution
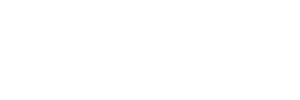
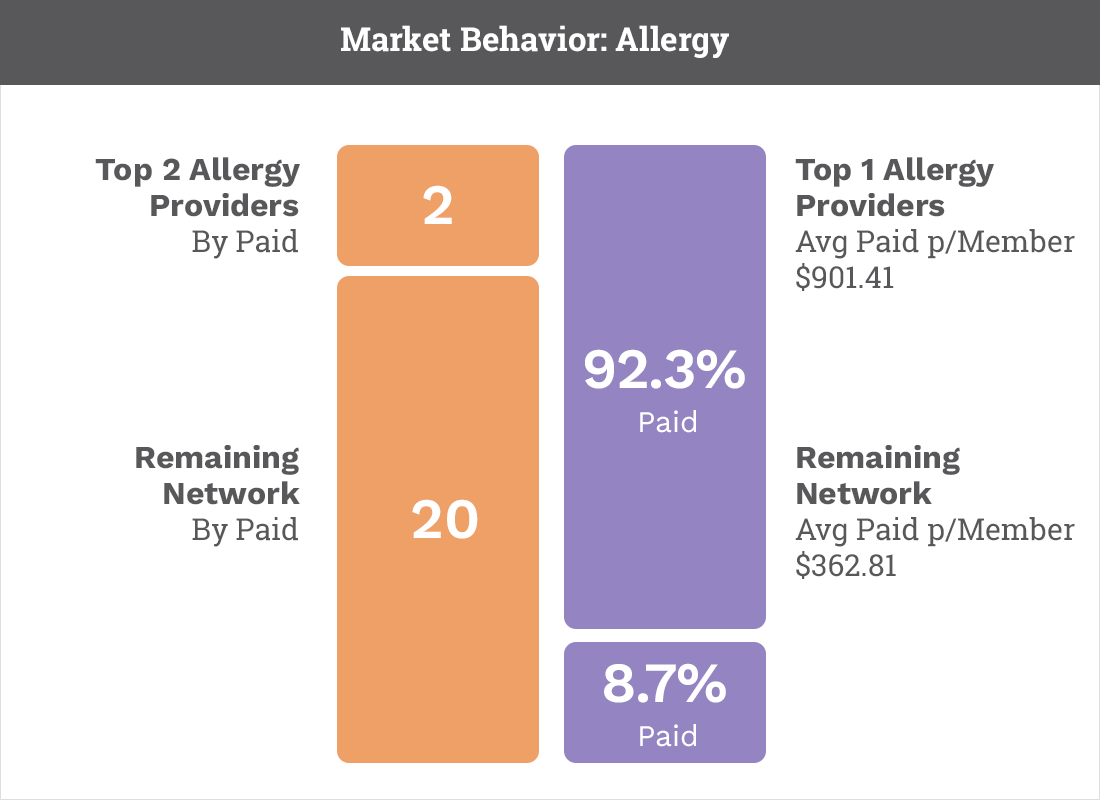
Leveraging claims data, FHG will map the potential clinical data “results” range across your clinical network.